“What do you guys do for wonky shoulder blades?” It’s a common question that comes up as we teach our Barbell Rehab Method Certification course around the country, and we wanted to take the time to create a solid resource to direct folks to. We could keep this blog short by simply answering, “eh.. we aren’t terribly concerned about scapular dyskinesis in most cases,” but we wanted to offer more nuance and explore some recent articles that have guided our journey to our current stance.
I would highly encourage anyone who has not already read our corrective exercise conundrum article to go ahead and dive into that one first, as it will give you a solid foundation to lead into the details of treating scapular dyskinesis (oftentimes referred to as scapular winging). Without further ado, let’s explore the current evidence behind all things scapular dyskinesis. Before we begin though, enjoy this photo of Dr. Ben’s scapulae. (Bonus points if you can guess correctly if he has shoulder pain!)

What is Scapular Dyskinesis?
Let’s begin with trying to define scapular dyskinesis. The scapula works with the humerus to produce movement at the shoulder joint. When we elevate our arm, we get varying degrees of three primary motions of the scapula: upward rotation, posterior tilting and external rotation.
As the humerus elevates, any decrease of these movements outside of the normal ratio is said to be “abnormal” movement or dyskinesia.
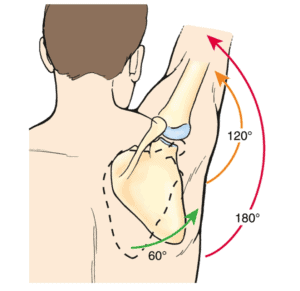
Supposedly "normal" scapulohumeral rhythm
What is “Normal” Scapulohumeral Rhythm Anyway?
When we begin looking at the research and what is truly “normal”, the water begins to muddy rather quickly. Numerous studies have looked at 3D kinematics of the scapula at rest and with movement in those with and without shoulder pain with greatly varying degrees of movement (1, 2, 3, 4, 5, 6). In addition, Lee et al 2013 showed that kinematics also changed based on if the subjects were performing functional tasks or simply moving their arms without weight as instructed by examiners.
This makes it difficult to extrapolate findings from laboratory studies measuring constrained movement versus scapular movement during more functional, everyday tasks.
Additionally, we run into further difficulty with “standardizing” scapular movement as demonstrated by this description of recent research conflicting with the idea of a “standard” 2:1 scapulohumeral rhythm:
“More recent studies have shown that scapulohumeral rhythm ranges from 1:1 to 6:1, depending on factors such as how kinematics are measured, the plane of elevation of the arm and whether there is an external load. Other factors that influence scapulohumeral rhythm include speed of motion, pain, shoulder tightness, and fatigue." (4)
These authors go on to emphasize that clinical observation of clinician deemed “abnormal scapular movement” should be held with extreme uncertainty of importance due to the high likelihood of the observed movement simply being on the spectrum of normal kinematic variation.
Can We Even Accurately Identify Scapular Dyskinesis?
Ellenbecker et at 2012 also looked at assessment of scapular dyskinesis and concluded there to be “low reliability of visual observation and classification of scapular movement.” (7)
Additionally, Plummer et al 2017 found,
“Scapular dyskinesis as assessed with the scapular dyskinesis test (SDT) is not more prevalent in those with shoulder pain. Rating was influenced by an examiner’s knowledge of shoulder pain presence. Scapular dyskinesis may represent normal movement variability.” (8)
“Influenced by an examiner’s knowledge of pain presence” is an important point I do not want to glance over. This is a common finding seen more and more often in research trials. This could be an entire blog in and of itself, but essentially, clinicians and researchers are great at finding what we are looking for.
If we believe scapular dyskinesis contributes to pain and a patient presents with shoulder pain, we will be much more likely to classify their shoulder blade as “dyskinetic”. This builds off of the concept of pareidolia: “the tendency to perceive a specific, often meaningful image in a random or ambiguous visual pattern.” (9) Common examples include seeing animal shapes in clouds or images in burnt pieces of toast.

Unnecessarily Generating “Dysfunctions”
Humans often have a tendency to try to create meaning from chaos or “noise”, and finding a “dysfunction” when someone is in pain is no different (10, 11). Hence the beauty of the Plummer et al 2017 article… they had two examiners independently assess for scapular dyskinesis, one who was blinded to whether the given participant had pain and one who was not. When the non-blinded researcher assessed for scapular dyskinesis, they found it in 80% of cases versus the blinded researcher who found it in only 67% (8).
When aware of pain, it is human tendency to be more generous in discovering “dysfunctions” such as scapular dyskinesis to make sense of the pain experience. However, as we will touch on, pain is always more complex than reducing the experience down to one “flaw”.
Overall, we do not have any consistent and conclusive data for what is “normal” positioning of the scapula, especially considering the vast variations seen depending on the task and associated demands (speed, weight, etc). Movement of the scapula is highly variable with extremely poor reliability of “assessment” and therefore should not be pathologized based on observation. However, the one caveat to this is what Adam Meakins calls the “vomit test”, where if you observe a scapula or movement that looks suspiciously atypical, we may want to consider neural pathology such as an accessory nerve or long thoracic nerve impairment.
Injury Risk and Scapular Dyskinesis
Okay, so we’re not great at measuring “normal” and will assign the label of “dyskinesis” more often when we know there is pain... Let’s say we ignore that and just classify a scapula with “dyskinesis” based on loser criteria. Does injury risk increase in those with scapular dyskinesis?
Struyf et al 2014 performed a prospective trial looking at exactly this and found no risk of future injury in overhead athletes based on scapular position and kinematics (12). In another prospective study by Hogan et al 2020 looking at 923 athletes, 54% had normal scapula control and 46% had dyskinesia (13). Out of those without dyskinesis, 21% went on to develop an injury and of those with dyskinesis, 25% went on to develop an injury, leading the authors to conclude that scapular dyskinesis in isolation does not predict future shoulder pain or injury.
Ratcliffe et al performed a systematic review in 2013 looking at potential relationships between subacromial “impingement” syndrome (SIS, now known as subacromial pain syndrome or (14) rotator cuff-related shoulder pain) and scapular orientation and concluded that “there is insufficient evidence to support a clinical belief that the scapula adopts a common and consistent posture in SIS.” (5) The authors went on to acknowledge the likelihood of this finding due to the multifactorial, complex nature of pain along with potential “methodological variations and shortfalls in the available research.” They also make a point that their findings “raise the possibility that deviation from a ‘normal’ scapular position may not be contributory to SIS but part of normal variations.”
Timmons et al in 2012 performed a meta-analysis looking for any potential relationship between subacromial pain and scapular kinematics and found a number of various kinematic changes (6). However, the kinematic changes found were inconsistent between populations of subjects (athletes versus overhead workers versus general population), further muddying the waters. The authors concluded that subjects with subacromial pain did indeed demonstrate altered scapular kinematics, but that the observed differences were all influenced and varied based on the plane of movement, level of arm elevation and patient population.
Let’s Give Scapular Dyskinesis the Benefit of the Doubt...
So, we have a study showing scapular dyskinesis in isolation does not predict future pain or injury, a meta-analysis showing some changes in scapular kinematics with pain (albeit highly variable between populations) and a systematic review showing no consistent changes in scapular kinematics or orientation with shoulder pain. (I’d be remissed not to again mention that Plummer et at 2017 also found scapular dyskinesis to be no more prevalent in those with shoulder pain than without.)
Let’s give scapular dyskinesis the benefit of the doubt and say maybe it is a risk factor for pain and/or maybe a byproduct of pain, even though the research does not support this. Does scapular dyskinesis have to change or “be fixed” for folks to get better?
Do We Need to “Fix” Scapular Dyskinesis?
Camargo et al 2015 put 46 folks with subacromial pain through either an exercise and stretching program or exercise, stretching and manual therapy program to see if their scapular kinematics had to change in order to get better. At this point, I hope you’re not surprised, but both groups got better without changes in scapular kinematics (15). This begs the question of what was the catalyst for recovery if scapular kinematics did not have to change?
It may be helpful to consider similar trials in the lumbar spine where low back pain improved without the transverse abdominis firing timing “normalizing” or multifidus musculature intersegmentally hypertrophying (16, 17, 18). As is a theme we try to fully endorse at Barbell Rehab, pain is much more complex than any single factor and cannot be simply reduced down with simple mechanical explanations. Kinematics do not have to change in order to modify pain, although we fully endorse that can be one option to explore.
For example, Reijneveld et al in 2017 found that training the scapular musculature was effective in decreasing shoulder pain (19). Sturyf et al in 2012 performed a similar study but separated folks with shoulder pain into two treatment groups of either scapular focused treatment consisting of stretching and scapular motor control training or a control group performing stretching, muscle friction, and eccentric rotator cuff training. The scapular control group had significantly greater reductions in pain compared to the control group without altered scapular kinematics (20).
Don’t Throw the Baby Out With the Bathwater
Cumulatively, these studies demonstrate that treating the scapula can still be a great way to reduce shoulder pain, but it’s not because any “dyskinesis” is “corrected”. The recent SExSI trial also showed that folks with shoulder pain got better (51% reached the Patient Acceptable Symptom State) even though they didn’t get stronger, demonstrating strength is also not a necessary factor needing to be changed to decrease pain (21, 22). Pain is complex and multifactorial, which gives us many factors to target to manage successfully.
When it comes to “wonky” or "winged" shoulder blades, “don’t miss the forest for the trees”. Spending too much time analyzing and drawing attention to scapular kinematics can keep you busy focusing on minutia that are likely far less important than guiding the patient/client in front of you back to their meaningful activities.
It’s certainly advantageous to train all of our scapular musculature from many standpoints (physical activity guidelines, movement variability, exercise induced hypoalgesia) which can make it worthwhile, but “correcting faulty scapular kinematics” need not be part of our narrative while coaching our clients/patients.
It is also not absurd to consider scapular dyskinesis to be a potentially positive adaptation for some folks depending on their sport, as they would likely have increased range of motion in certain planes and could leverage different length-tension relationships between scapular muscles as mentioned by some authors (4, 23). As discussed in The Corrective Exercise Conundrum, comprehensive capacity, or the overall human’s ability to tolerate various loads necessary for the demands of their valued activities should be of top priority (36). It can still be beneficial to train all scapular muscles, but there is rarely anything that inherently needs correcting.
Tying it All Together
So, there you have it! How do we treat scapular dyskinesis or scapular winging? We don’t worry about it much unless we are concerned of potential nerve injury or obvious performance implications. Time can often be better spent targeting comprehensive capacity and programming geared towards the client/patient’s specific meaningful activities and goals. And for those still concerned, Dr. Ben does not have shoulder pain 🙂
References
- Lee SK, Yang DS, Kim HY, Choy WS. A comparison of 3D scapular kinematics between dominant and nondominant shoulders during multiplanar arm motion. Indian J Orthop. 2013;47:135–142.
- Ludewig PM, Reynolds JF. The association of scapular kinematics and glenohumeral joint pathologies. J Orthop Sports Phys Ther 2009;39:90–104.
- McClure et al. Shoulder function and 3-dimensional kinematics in people with shoulder impingement syndrome before and after a 6-week exercise program. Phys Ther. 2004 Sep;84(9):832-48.
- McQuade et al. Critical and Theoretical Perspective on Scapular Stabilization: What Does It Really Mean, and Are We on the Right Track? Phys Ther. 2016 Aug;96(8):1162-9.
- Ratcliffe E, Pickering S, McLean S, et al. Is there a relationship between subacromial impingement syndrome and scapular orientation? A systematic reviewBritish Journal of Sports Medicine 2014;48:1251-1256.
- Timmons, M. K., Thigpen, C. A., Seitz, A. L., Karduna, A. R., Arnold, B. L., & Michener, L. A. (2012). Scapular Kinematics and Subacromial-Impingement Syndrome: A Meta-Analysis, Journal of Sport Rehabilitation, 21(4), 354-370.
- Ellenbecker T, Kibler W, Bailie D, Caplinger R, Davies G, & Riemann B (2012). Reliability of scapular classification in examination of professional baseball players. Clinical Orthopaedics and Related Research, 470, (6) 1540-1544.
- Plummer et al. Observational Scapular Dyskinesis: Known-Groups Validity in Patients With and Without Shoulder Pain. J Orthop Sports Phys Ther. 2017 Aug;47(8):530-537.
- Merriam-Webster. (n.d.). Pareidolia. Merriam-Webster. Retrieved October 1, 2021, from https://www.merriam-webster.com/dictionary/pareidolia.
- Burton, R. A. (2009). On being certain: Believing you are right even when you're not. St. Martin's Griffin.
- Hallinan, J. T. (2010). Why we make mistakes: How we look without seeing, forget things in seconds, and are all pretty sure we are way above average. Broadway Books.
- Struyf, F.; Nijs, J.; Meeus, M.; Roussel, N.A.; Mottram, S.; Truijen, S.; Meeusen, R. Does scapular positioning predict shoulder pain in recreational overhead athletes? Int. J. Sports Med. 2014, 35, 75–82.
- Hogan C, Corbett JA, Ashton S, Perraton L, Frame R, Dakic J. (2020). Scapular Dyskinesis Is Not an Isolated Risk Factor for Shoulder Injury in Athletes: A Systematic Review and Meta-analysis. The American Journal of Sports Medicine, 036354652096850.
- Lewis, J. (2018). The End of an Era? Journal of Orthopaedic & Sports Physical Therapy, 48(3), 127–129. doi:10.2519/jospt.2018.0102
- Camargo, P. R., Alburquerque-Sendín, F., Avila, M. A., Haik, M. N., Vieira, A., & Salvini, T. F. (2015). Effects of Stretching and Strengthening Exercises, With and Without Manual Therapy, on Scapular Kinematics, Function, and Pain in Individuals With Shoulder Impingement: A Randomized Controlled Trial. Journal of Orthopaedic & Sports Physical Therapy, 45(12), 984–997. doi:10.2519/jospt.2015.5939
- Mannion AF, Caporaso F, Pulkovski N, Sprott H. Spine stabilisation exercises in the treatment of chronic low back pain: a good clinical outcome is not associated with improved abdominal muscle function. Eur Spine J. 2012 Jul;21(7):1301-10. doi: 10.1007/s00586-012-2155-9. Epub 2012 Jan 24. PMID: 22270245; PMCID: PMC3389103.
- Vasseljen O, Unsgaard-Tøndel M, Westad C, Mork PJ. Effect of core stability exercises on feed-forward activation of deep abdominal muscles in chronic low back pain: a randomized controlled trial. Spine (Phila Pa 1976). 2012 Jun 1;37(13):1101-8. doi: 10.1097/BRS.0b013e318241377c. PMID: 22146280.
- Wong AY, Parent EC, Funabashi M, Kawchuk GN. Do changes in transversus abdominis and lumbar multifidus during conservative treatment explain changes in clinical outcomes related to nonspecific low back pain? A systematic review. J Pain. 2014 Apr;15(4):377.e1-35. doi: 10.1016/j.jpain.2013.10.008. Epub 2013 Nov 1. PMID: 24184573.
- Reijneveld et al. Clinical outcomes of a scapular-focused treatment in patients with subacromial pain syndrome: a systematic review. Br J Sports Med. 2017 Mar;51(5):436-441.
- Struyf F, Nijs J, Mollekens S, Jeurissen I, Truijen S, Mottram S, & Meeusen R (2012). Scapular focused treatment in patients with shoulder impingement syndrome: a randomized clinical trial. Clinical Rheumatology, 32, (1) 73-85.
- Clausen MB, Hölmich P, Rathleff M, et al. Effectiveness of Adding a Large Dose of Shoulder Strengthening to Current Nonoperative Care for Subacromial Impingement: A Pragmatic, Double-Blind Randomized Controlled Trial (SExSI Trial). The American Journal of Sports Medicine. 2021;49(11):3040-3049. doi:10.1177/03635465211016008
- Powell JK, Lewis JS. Rotator Cuff-Related Shoulder Pain: Is It Time to Reframe the Advice, "You Need to Strengthen Your Shoulder"? J Orthop Sports Phys Ther. 2021 Apr;51(4):156-158. doi: 10.2519/jospt.2021.10199. PMID: 33789431.
- Littlewood et al. Scapular dyskinesis and shoulder pain: the devil is in the detail. Br J Sports Med 2018;52:72-73.
- Burn, M. B., McCulloch, P. C., Lintner, D. M., Liberman, S. R., & Harris, J. D. (2016). Prevalence of Scapular Dyskinesis in Overhead and Nonoverhead Athletes: A Systematic Review. Orthopaedic journal of sports medicine, 4(2), 2325967115627608. https://doi.org/10.1177/2325967115627608
- Bury et al. Effectiveness of scapula-focused approaches in patients with rotator cuff related shoulder pain: A systematic review and meta-analysis. Man Ther. 2016 Sep;25:35-42.
- Giuseppe, L.U., Laura, R.A., Berton, A., Candela, V., Massaroni, C., Carnevale, A., Stelitano, G., Schena, E., Nazarian, A., DeAngelis, J., & Denaro, V. (2020). Scapular Dyskinesis: From Basic Science to Ultimate Treatment. International Journal of Environmental Research and Public Health, 17.
- Hickey et al. Accuracy and reliability of observational motion analysis in identifying shoulder symptoms. Man Ther. 2007 Aug;12(3):263-70.
- Hickey et al. Scapular dyskinesis increases the risk of future shoulder pain by 43% in asymptomatic athletes: a systematic review and meta-analysis. Br J Sports Med. 2018 Jan;52(2):102-110.
- Hotta, G. H., Santos, A. L., McQuade, K. J., & de Oliveira, A. S. (2018). Scapular-focused exercise treatment protocol for shoulder impingement symptoms: Three-dimensional scapular kinematics analysis. Clinical Biomechanics, 51, 76–81. doi:10.1016/j.clinbiomech.2017.12.005
- Jones et al. Training Load and Fatigue Marker Associations with Injury and Illness: A Systematic Review of Longitudinal Studies Sports Med (2017) 47: 943.
- Kibler et al. Clinical implications of scapular dyskinesis in shoulder injury: the 2013 consensus statement from the ‘Scapular Summit’. Br J Sports Med. 2013 Sep;47(14):877-85.
- Kibler WB, Ludewig P, McClure P, Michener L, Bak K, Sciascia (2013). Clinical implications of scapular dyskinesis in shoulder injury: the 2013 consensus statement from the ‘scapular summit.’ British Journal of Sports Medicine. Published online first: April 18, 2013 as 10.1136/bjsports-2013-092425.
- Kibler WB, McMullen J (2003). Scapular dyskinesis and its relation to shoulder pain. Journal of the American Academy of Orthopaedic Surgeons, 11(2), 142-51.
- Lange et al. The reliability of physical examination tests for the clinical assessment of scapular dyskinesis in subjects with shoulder complaints: A systematic review. Physical Therapy in Sport, 26, 64–89.
- Lauersen JB, Bertelsen DM, Andersen LB. The effectiveness of exercise interventions to prevent sports injuries: a systematic review and meta-analysis of randomised controlled trials. Br J Sports Med. 2014;48(11):871-877.
- Lehman, G. (2017, January 9). Comprehensive Capacity: An Alternative to the Kinesiopathologial Model for Shoulder Function [web log]. Retrieved September 15, 2021, from this article.
- Lehman, G. (2015, August 3). Functional exercise is a poor term- how about some comprehensive capacity. [web log]. Retrieved September 15, 2021, from this article.
- Lucasiewicz A, Pratt N, Sennett B, McClure P, & Michener L (1999). Comparison of 3-dimensional scapula position and orientation between subjects with and without shoulder impingement. Journal of Orthopaedic and Sports Physical Therapy, 29, (10) 574-586.
- Madsen et al. Training Induces Scapular Dyskinesis in Pain-Free Competitive Swimmers: A Reliability and Observational Study. Clinical Journal of Sport Medicine, 21(2), 109–113.
- Maenhout et al. “Acromiohumeral Distance and 3-Dimensional Scapular Position Change After Overhead Muscle Fatigue.” Journal of Athletic Training 50.3 (2015): 281–288.
- Morais N & Pascoal A (2013). Scapular positioning assessment: Is side-to-side comparison clinically acceptable? Manual Therapy, 18, (1) 46-53.
- Nijs J, Roussel N, Vermeulen K and Souvereyns G. Scapular positioning in patients with shoulder pain: a study examining the reliability and clinical importance of 3 clinical tests. Arch Phys Med Rehabil 2005; 86: 1349–55.
- Rich et al. “Scapular Upward-Rotation Deficits After Acute Fatigue in Tennis Players.” Journal of Athletic Training 51.6 (2016): 474–479.
- Shadmehr A, Bagheri H, Ansari N, & Sarafraz H (2010). The reliability measurements of lateral scapula slide test at three different degrees of shoulder abduction. British Journal of Sports Medicine, 44, 289-293.
- Tate et al. A clinical method for identifying scapular dyskinesis, part 2: validity. J Athl Train 2009;44:165–73.
- Takeno, K., Glaviano, N.R., Norte, G.E., & Ingersoll, C.D. (2019). Therapeutic Interventions for Scapular Kinematics and Disability in Patients With Subacromial Impingement: A Systematic Review. Journal of athletic training, 54 3, 283-295.
- Turgut et al. Effects of Scapular Stabilization Exercise Training on Scapular Kinematics, Disability, and Pain in Subacromial Impingement: A Randomized Controlled Trial. Archives of Physical Medicine and Rehabilitation. 2017; 98(10), 1915–1923.e3.
- Willmore et al. “Scapular Dyskinesia: Evolution towards a Systems-Based Approach.” Shoulder & Elbow 8.1 (2016): 61–70.
- Wright et al. Diagnostic accuracy of scapular physical examination tests for shoulder disorders: a systematic review. Br J Sports Med. 2013 Sep;47(14):886-92.





