In today’s unfortunately ego-driven world, everyone wants to be “that person” who “fixes” someone else, and this can lead to a divide between fitness and rehab professionals. Strength coaches and personal trainers may be hesitant to refer out to a physical therapist because “what does he or she know about lifting weights,” and physical therapists become weary to recommend personal training after a client finishes therapy in fear that the trainer might “undo” everything with poor exercise selection or programming.
I think this needs to change. My name is Dr. Michael Mash, and I have a passion for uniting the fitness and rehab industries in order to maximize client outcomes!
The Unicorn Client
For fitness professionals: How often do you work with someone that has perfect mobility, no history of past injuries, and no current aches or pains? I’d be willing to bet that this unicorn client is VERY rare to find. The truth is, we are all human, and the majority of the clients you work with probably have SOMETHING going on that you need to work around.
This can often lead to a gray area of fitness professionals not knowing if or when to refer out to a rehab specialist. You may not want to refer out for something that can be easily handed on your own; but, you also shouldn’t be performing a comprehensive rehab program in the gym. Where do we draw the line?
Let’s Start with Red Flag Symptoms

One way to know for sure that you should refer someone out for immediate medical attention, is the presence of red flags. Red flags are signs or symptoms that indicate that the client may be experiencing a more serious underlying medical condition. Examples of these may include, but not limited to:
- Chest pain that worsens with exertion
- Onset of weakness, numbness, or inability to move a limb
- Difficulty speaking, confusion, unsteadiness, or difficulty walking
- Severe abdominal pain
- Severe headache, blurred vision, or loss of vision
- Difficulty controlling bowel or bladder
- Numbness or shooting pain down both legs
- Changes in sensation around the genital region
- Unplanned significant weight loss.
If your client is experiencing one of these, this is NOT something you should mess around with. Refer them out to a medical provider. Now that I’m done scaring you with all of the horrible things that could go wrong, the good news is this: If they’re NOT experiencing one of the symptoms listed above, it’s most likely not something of imminent medical concern.
But What About Pain with Movements?
So you’ve done your due diligence and ruled out any red flags, and it’s time to perform your initial movement assessment with your client. Everyone does this differently, but most of the time it includes some sort of bodyweight squat, hinge, and lunge pattern for the lower body, and then some sort of overhead reaching movement.
What do you do if they have pain with one of these? Do you immediately refer out? Do you ignore it?
Like we mentioned with our unicorn client, the odds are low that someone will present with absolutely zero mobility limitations or aches and pains. Should you send them into the medical model if they don’t “pass” your screen? Keep reading.
Don’t Fit a Square Peg into a Round Hole
Everyone is built differently. Let’s use hip structure as an example. When it comes to hip anatomy, people will display different degrees of version, or the way the femoral neck is rotated relative to the femoral condyles (knee).
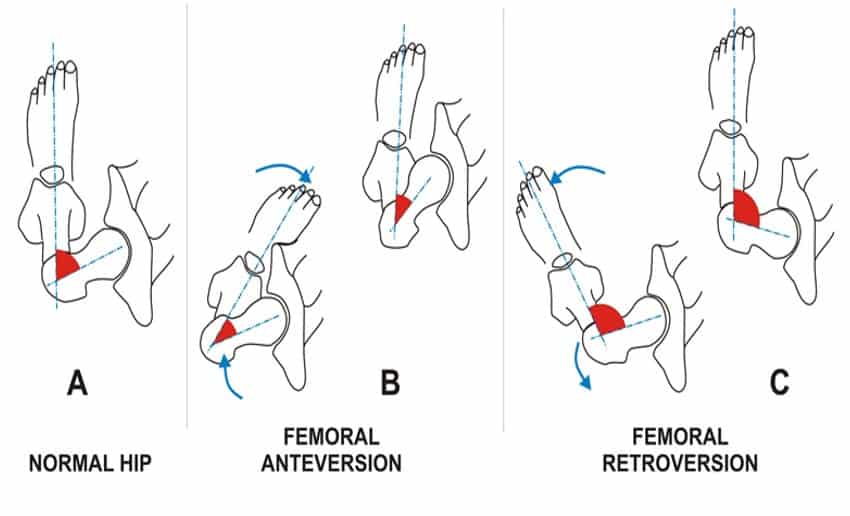
Some may be retroverted (rotated outward) and some may be anteverted (rotated inward). This degree of version will correlate with someone’s squat stance.
In general, those with excessive retroversion will feel more comfortable with their toes turned OUT during the squat, and those with more anteversion will feel better with their toes pointed more forward. More on that here.
What happens if you take a highly retroverted individual and try to fit them into a narrow stance, toes forward squat? It doesn’t feel that great. It may cause a pinching sensation in the front of the hip or even pain. Do you need to refer out for this? Probably not yet, as the pain or pressure can usually be eradicated by just moving their stance out or turning their toes out.
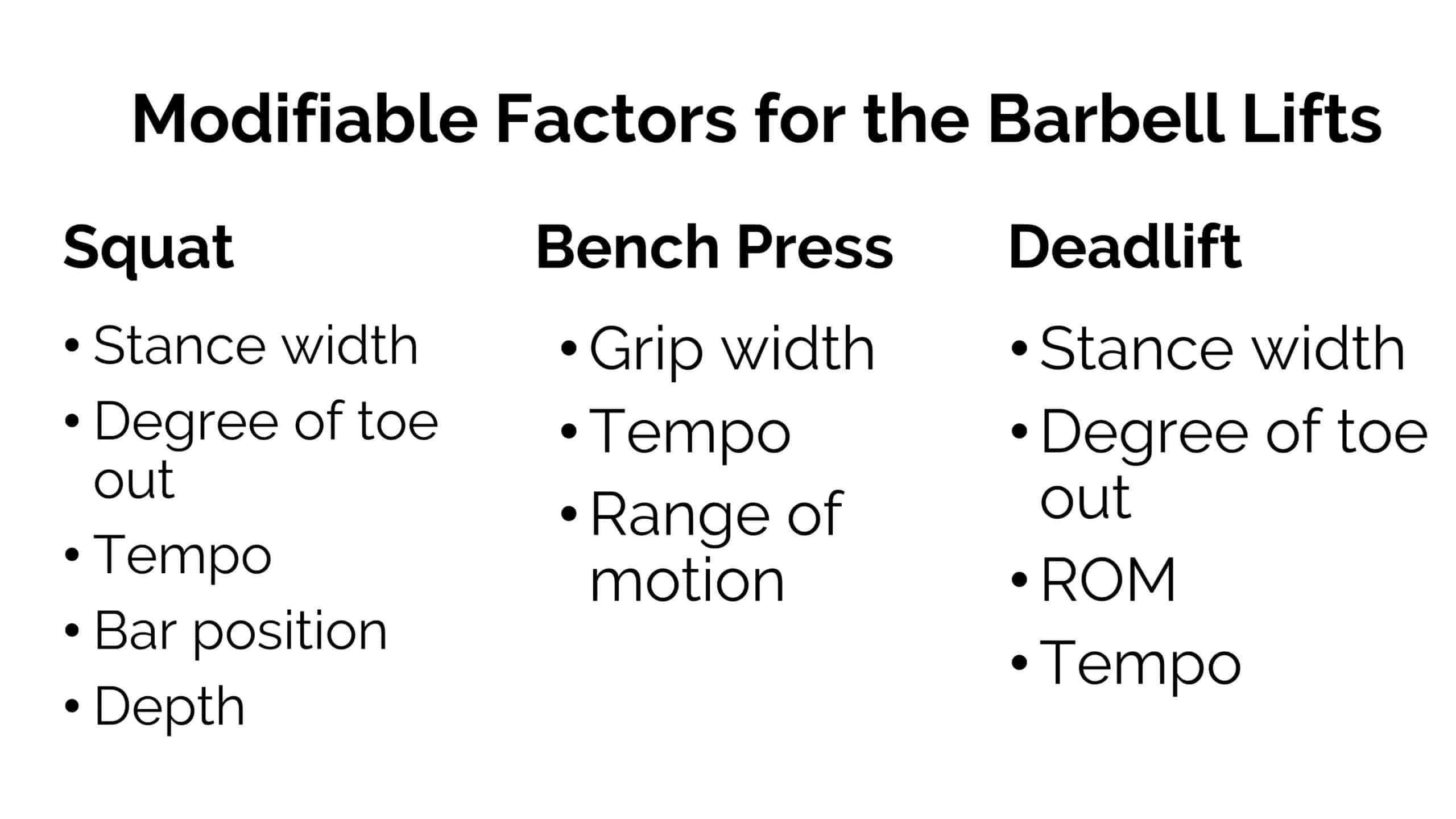
So as you can see by our example, anatomy may dictate why someone would feel better with one form variation vs. another. If all it takes is a simple form adjustment to make a lift or a movement feel more comfortable, then that’s usually something you can take care of, on the spot, right in the gym. Here are a list of form adjustments, or modifiable factors you can experiment with for each lift:
Fore more information on how to overcome hip pain during squats, head here.
Dosage Matters Too
Let’s use another example. A client comes to you for an initial assessment and mentions that he has some nagging shoulder pain. After learning about his prior training history, you find out the following. He:
- Bench presses 3x/week for high volume (3-4 x 12-15 reps) taking each set to failure
- Doesn’t include any horizontal rowing or scapular retraction exercises
- Doesn’t do any type of movement prep or warm-up and doesn’t warm up with lighter weights on the bench press.
Here’s the truth. No amount of manual therapy, foam rolling, trigger point release, or massage gun is going to fix this issue. This is a programming error. As a strength coach or personal trainer, this is your wheelhouse. You are equipped with the knowledge of how to optimize programming for this client.
There is a good chance, in fact, that his shoulder pain would probably go away if you optimized his programming. So maybe you change it to the following:
- Bench press two times a week. Keeping the RPE of the working sets between 7 and 8.5
- Adding in some accessory horizontal rowing variations for 3 x 10-12 reps at RPE 8
- Making sure he starts with the empty barbell on the bench press and performs warm-ups sets prior to hitting his working weights.
Optimizing programming can do wonders for reducing someone’s pain, and as exercise experts, it’s within your scope to do this. You’re not “treating” the pain. You’re simply optimizing the dosage.
When Form and Programming Optimization Doesn’t Work
Sometimes even after optimizing or modifying form, and dialing in the programming, someone may still have pain. This is the prime opportunity to refer the client out to a trusted rehabilitation expert for further assessment and treatment.
This is, where I believe, the line should be drawn between fitness and rehabilitation. In other words, you don’t want to refer out for issues that can be easily fixed with adjusting form or programming, but you also don’t want to be trying to play physiotherapist either. This is why local networking is so key! Every fitness professional should know a few good rehab professionals in their local area, and vice versa.
But I Have a Bulging Disc…I Can’t Deadlift

Let’s talk about another scenario that happens quite often. This is the case of a client who may have had history of back pain, feels good now, but is afraid to have it again. She might even bring an MRI to her initial fitness consult or tell you something along the lines of this:
“I have history of back pain. Look at my MRI. It shows a few disc bulges in my low back, so I definitely shouldn’t be doing deadlifts.”
What do you do? Can you prescribe deadlifts for someone that has disc bulges? The answer is…it depends.
Here’s the truth. 40% of 30 year olds with NO back pain, will show a disc bulge on MRI. This number then increases to 50% of 40 years (1). Yes you heard that correctly. Take someone in their 40s with zero back pain and flip a coin. There’s a heads/tails chances that they have a disc bulge in their lumbar spine without even knowing about it. This is a prime opportunity to provide this type of education to the client. We can normalize these things as “wrinkles on the inside.”
If they aren’t currently experiencing any red flag symptoms (Iisted in the beginning of the article), aren’t experiencing any significant back pain, and don’t have any radicular symptoms (pain/numbness shooting down a leg), then you can proceed forward with intelligent lower body programming.
Find a hip hinging variation that they can tolerate and enjoy doing (conventional deadlift, sumo deadlift, trap bar deadlift) and have at it! If they have a few disc bulges on an MRI but aren’t currently symptomatic, working out and loading the lower body will help increase strength and build some psychological resiliency too. Showing someone that they aren’t as “broken” or “weak” as they think they are is one of the most empowering things you can do for someone.
The Big Picture
My goal with Barbell Rehab is to unite the fitness and rehab communities in order to maximize client outcomes. In a world today filled with over-medicalization and opioid abuse, if we can work TOGETHER to keep people healthy, strong, and enjoying life to the fullest, that’s one hell of a rewarding feeling.
As a strength coach or personal trainer, it is rare that you will come across a client who has perfect mobility or zero pain (after all, we are human) so here’s what you should do:
- First, optimize the programming. Make sure the client is warming up efficiently for each lift and the majority of their working sets are performed in the RPE 7-8.5 range.
- Second, optimize and modify the form. If they have discomfort or pain with a certain lift, see if you can “tweak” it a bit by changing the stance width, degree of toe out, grip width, etc.
- If the client still has pain after form and programming optimization, refer out to a trusted rehab specialist.
It shouldn’t be fitness professional vs. rehab specialist. Instead, lets team up to fight over-medicalization TOGETHER!
(1) Brinjikji W, Luetmer PH, Comstock B, et al. Systematic literature review of imaging features of spinal degeneration in asymptomatic populations. AJNR Am J Neuroradiol. 2015;36(4):811-6.





